Amid Cough Syrup Deaths, Big Reveal In Centre’s 2024 Audit On Drug Testing
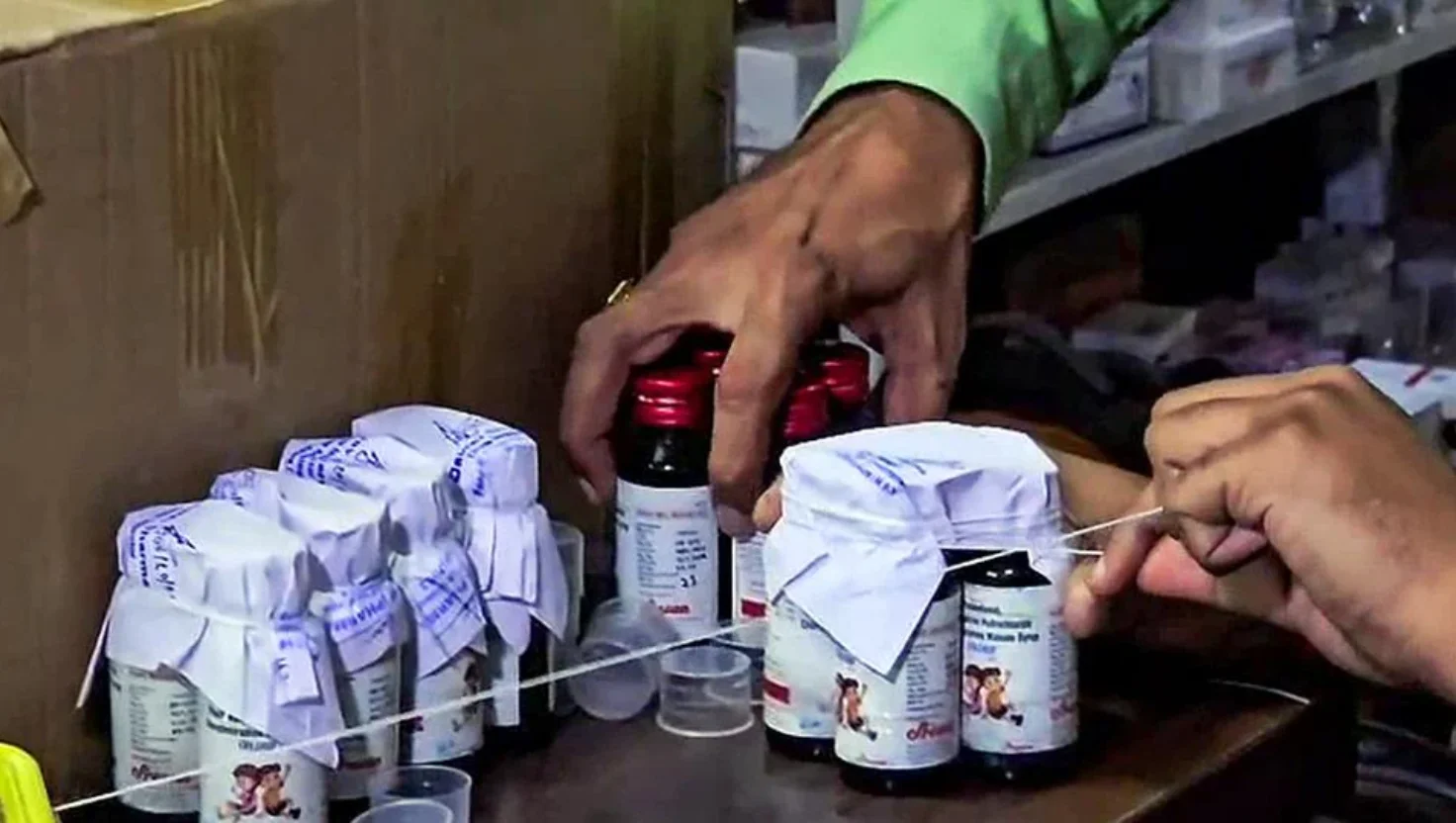
In the aftermath of multiple international incidents linking Indian-made cough syrups to child deaths abroad, the Centre’s 2024 audit on drug testing laboratories has revealed serious flaws in the country’s pharmaceutical quality control system. The findings expose a troubling picture — one where inadequate infrastructure, outdated equipment, and inconsistent testing practices have undermined India’s reputation as the “pharmacy of the world.”
The audit, commissioned by the Union Health Ministry and conducted across central and state drug testing facilities, was aimed at assessing compliance, capacity, and efficiency within India’s vast drug regulatory network. What it found, however, was an alarming pattern of non-uniform testing standards, manpower shortages, and lack of modern technology in several state-run labs.
Gaps in Oversight and Infrastructure
The 2024 audit found that only a limited number of laboratories across the country are equipped to carry out full-spectrum testing of pharmaceutical formulations. Many state drug control departments lack advanced analytical equipment such as gas chromatography or mass spectrometry tools — essential for detecting contaminants and toxic substances in medicines.
In several states, auditors reported inadequate sample testing and delayed results, often stretching for weeks due to low staff strength and outdated processes. Some labs were found operating with unfilled technical positions, leaving critical drug samples either untested or insufficiently examined before release into the market.
A senior official involved in the review reportedly noted that while India has over 8,000 drug manufacturing units, the number of functional, accredited testing laboratories remains strikingly small — putting immense pressure on a few central facilities. This imbalance, combined with procedural inefficiencies, leaves ample room for substandard or contaminated drugs to escape regulatory scrutiny.
The Global Fallout
The audit findings come on the heels of international scrutiny following reports from countries like Gambia, Uzbekistan, and Cameroon, where Indian-manufactured cough syrups were linked to tragic child deaths. These incidents, which drew global condemnation and warnings from the World Health Organization, placed a spotlight on India’s pharmaceutical export quality control.
While the government took immediate steps to suspend certain manufacturing licenses and mandate stricter export testing norms, the latest audit underscores a deeper, systemic weakness. The report suggests that the existing framework for quality assurance is reactive rather than preventive, responding to crises after they occur instead of proactively identifying risks.
Testing Bottlenecks and Human Resource Deficit
The audit paints a concerning picture of the human resource landscape in drug regulation. Many laboratories are functioning with skeletal staff, forcing them to prioritize only a small portion of the drug samples received for testing. Technical training and professional development for analysts are also found lacking in most states.
Moreover, auditors noted that data management and digital integration remain outdated, with several labs still depending on manual record-keeping. This hampers traceability, slows reporting, and increases the risk of human error in analysis.
Read more: No Remorse, No Responsibility’: Madras HC Slams Vijay Party Over Stampede
Experts suggest that the absence of a unified national database to track and flag quality violations across states has further complicated the regulatory ecosystem. Without interconnectivity between state and central labs, information silos prevent timely intervention when a defective batch is detected in one region.
Government’s Next Steps
Following the audit revelations, the Health Ministry is reportedly drafting an action plan to overhaul the drug testing infrastructure. Proposed measures include upgrading laboratories with modern analytical tools, introducing digital reporting platforms, and increasing staff recruitment and training programs.
There are also discussions about expanding the role of private NABL-accredited laboratories to support government facilities in sample testing, especially for exports. The Centre is expected to issue fresh guidelines mandating pre-export quality certification for all pharmaceutical consignments.
These reforms aim to rebuild global trust in India’s pharmaceutical exports, which account for over 20 percent of the world’s generic drug supply.
A Wake-Up Call for India’s Drug Ecosystem
The 2024 audit serves as a stark reminder that India’s pharmaceutical success story cannot rest on manufacturing scale alone — it must be backed by robust, transparent, and accountable quality assurance systems. The tragic cough syrup incidents have not only cost lives but also dented India’s image as a reliable drug producer.
Read more: India Warns Pakistan: Avoid Aggression Over Sir Creek Dispute
For a nation aspiring to lead in healthcare innovation and exports, the audit’s findings are a call for urgent introspection. Strengthening drug testing infrastructure, empowering regulatory bodies, and adopting uniform testing standards across states are essential steps toward ensuring that no life is lost to preventable negligence in medicine quality control.
If acted upon decisively, the audit could mark a turning point — from crisis management to preventive vigilance — redefining how India ensures the safety of every pill, syrup, and tablet that reaches patients at home and abroad.